💲Billing
Revenue Cycle implementation in Fieldworker
Using Fieldworker for Managing Revenue Cycle
An agency planning to use the Fieldworker platform for managing their RCM process will have to complete the setup described below.
Subscribe to Billing in Fieldworker
Set up your agency credentials
Set up payers
Process for charge capture
Matching Prior Authorization to Encounters
Generating Claims from Encounters
Upload/Generate claims
Submit Claims
Payer
In healthcare, a payor is a person, organization, or entity that pays for the care services administered by a healthcare provider. This term most often refers to health insurance companies, which provide customers with health plans that offer cost coverage and reimbursements for medical treatment and care services. Each time a healthcare provider submits a medical claim to a payor to receive reimbursement for a specific procedure or service, they generate information about that care episode.
Before a claim can be submitted to a payer, the payer should be defined and set up in the Fieldworker platform.

Once a payer is set up, its details are viewable on the settings page.

Once a new payer is added by an agency, the system generates an email to the Fieldworker support team notifying the same and follows up the completion of the setup with the payer.
Setting up the link with the payer is a mandatory step, generally executes outside the Fieldworker platform, and may take several days to complete.
Accounts Receivable dashboard
Accounts Receivable has an estimate of all expected revenue based on the data within the Fieldworker system.
shows the expected receivables based on the client population and the status of their plans.
The entries are always up to date, so changes are automatically reflected after each change, either manually or via DDD synch
Prior Auth status could be manually updated to indicate if this receivable is via submission for voucher payments
Payment status is updated when remittance advice is received from your payers. This can be also updated manually for recording voucher payments.
The Billing admins can also add notes to share context about payments and/or receivables etc.
The accounts receivable details for prior months may be viewed by adjusting the dates.

Prior Auth Dashboard
The prior auth dashboard has the entries uploaded from the prior auth file. This data can not be manually updated.
The prior auth entries are not editable
The dashboard also shows the matching tasks and associated MT, if any
The dashboard allows the admin users to create entries for subsequent claims submission.
The exact matching logic is described below
the general expectation here is that PA entries are what you can get paid for, and if there is a matching task with an 'Approved' MT, a claim may be created.
there is no additional logic to auto-generate the claims from this screen
are claim status, error code, and error description fields populated here?

You upload the prior auth file by clicking on the “Upload Pre-Auth CSV” in the top right of this screen (under Billing and “Charge Capture” from the side panels).
Under “Prior Authorization”, you can see any task that will need an MT to be filed. All the other information regarding the client will be pre-filled from data from the iRecord import, including the prior authorization number and service number.
Charge capture Dashboard
The goal here is to catch the changes in the prior auth file ... for prior periods. Under “Changes Captured”, you’ll see any changes made from the previous month when uploading your pre-authorization.

PA file has rolling 12 months of data .. and generally has changes in the prior periods that may have happened after the last month's PA file was generated
among the changes identified here
new customer, assigned after the last PA file
change in plan, after the last PA file
customer leaving, after the last PA file
for all changes captured with matching task and approved MT, a claim can be generated
almost in all cases, it will be one or more partial claims, to be submitted
are claim status, error code, and error description fields populated here?
in cases, where a claim may be already in place, it may need to be withdrawn
in some cases, there may be additional rules that may be needed, when a new client is added, etc. (this may not yet be in place)
Billing claims are created through the prior authorization form you receive from the DDD at the start of every month.
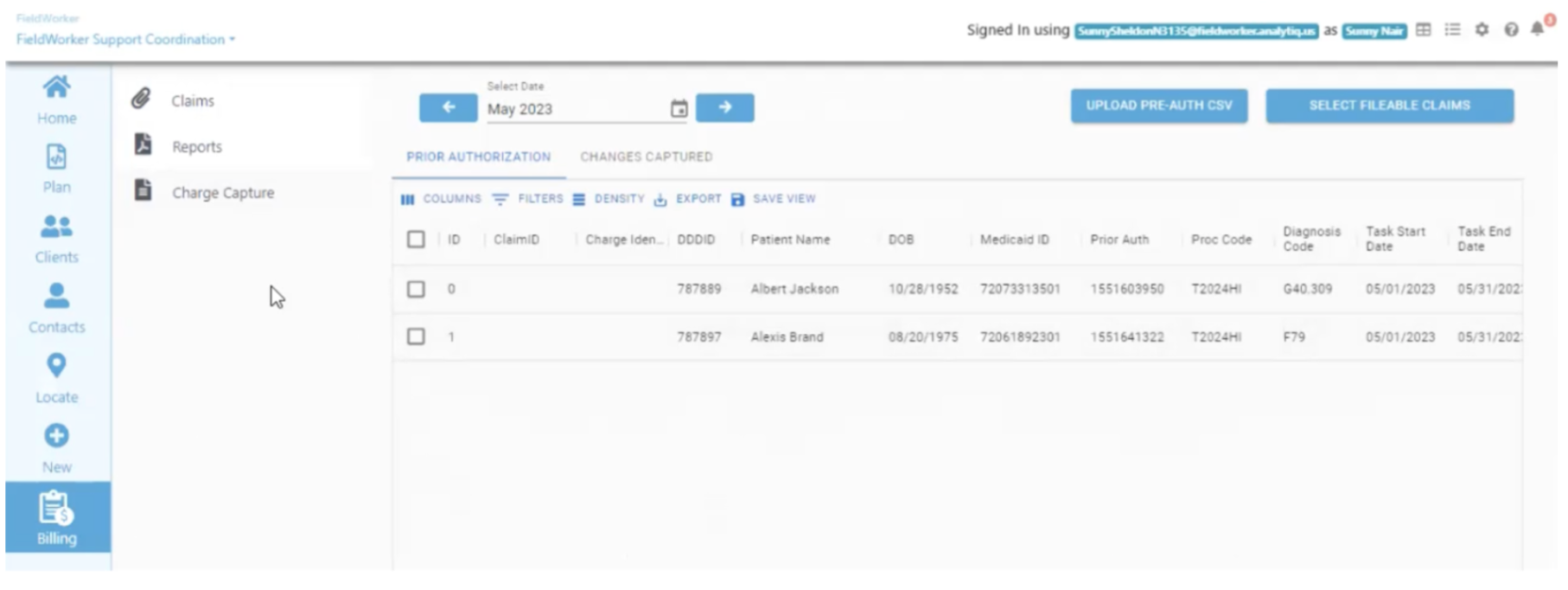
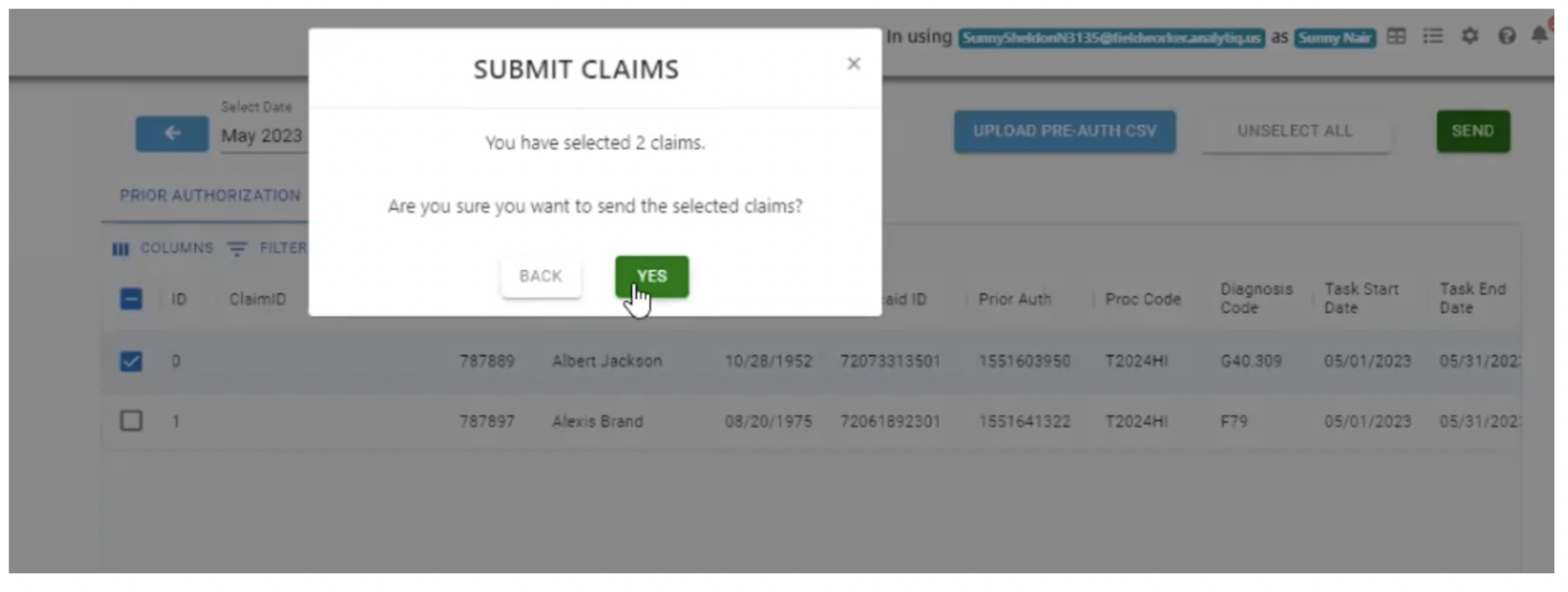
To submit a claim, select the relevant claims using the checkbox, click on “Select fillable claims”, followed by “Send”.
Claims Dashboard
shows the claims uploaded either via file upload or through Charge capture
allows to add manual claims, where needed
claims are run through some validations and some fields are allowed to be edited, before EDI file generation
post submission, this dashboard also shows the status and response from the billing agency, if any.
Once these claims have been filed, they’ll be displayed in the “Claims” table:
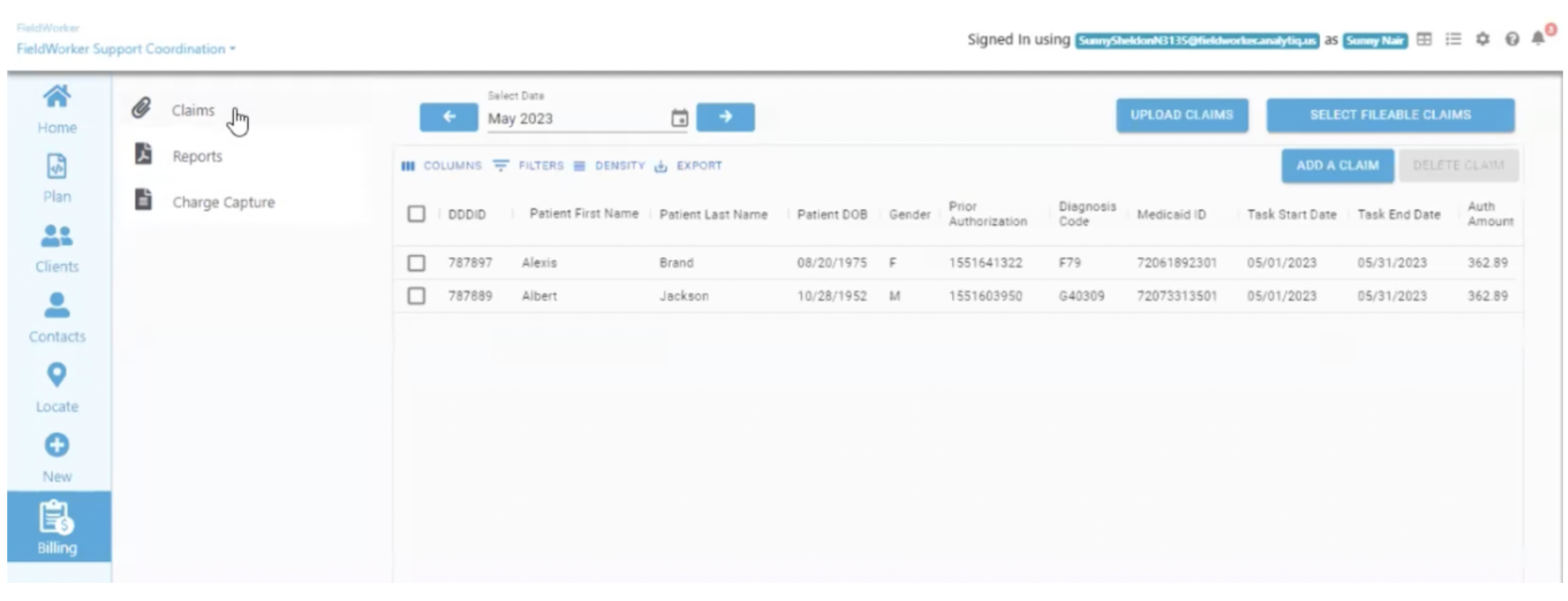
Under “Claim Status”, you’ll now see that these are “Ready to bill”, and can be submitted for billing.
Remittances Dashboard
The remittance dashboard is one place to see all your remittances received from Medicaid, even if they have not been submitted via the Fieldworker. The data in this dashboard is populated once the weekly remittance file from Medicaid is processed.
Procedure Code
Procedure_code – This is the master table containing details about all procedures that are eligible (or mandated) in a given state. These procedure codes are mapped to various tasks in the Fieldworker. The relevant tasks that are mapped to procedures performed by the company, should be appropriately selected in dropdown settings/configuration.
[procCode_id] [int] IDENTITY(1,1) NOT NULL,
[procCode] [varchar](24) NULL,
[procCode_description] [varchar](100) NOT NULL,
[procUnitOfService] [varchar](20) NOT NULL,
[procProcCode] [varchar](50) NOT NULL,
[procModifierCode] [varchar](20) NULL,
[procTaskType] [varchar](50) NULL,
[procIsActive] [int] NULL,
[addedBy] [varchar](50) NULL,
[addedOn] [datetime] NULL,
[procBaseTier] [varchar](10) NULL
Billing Rates
Billing rates – This is a master schedule of all billing rates paid for by Medicaid. This will mostly be available as report/lookup data.
[billingrate_id] [int] IDENTITY(1,1) NOT NULL, PK
[procProcCode] [varchar](50) NULL, FK
[tier] [varchar](10) NULL,
[rate] [decimal](5, 2) NULL,
[comp_id] [int] NULL, FK
[added_by] [varchar](50) NULL,
[added_on] [datetime] NULL
Payer
Payer – This is the master table containing details about all payers that are eligible or mandated in a given state.
[payer_id] [int] IDENTITY(2000,1) NOT NULL, PK
[payer_name] [varchar](150) NOT NULL,
[payer_is_active] [bit] NULL,
[payerTaxID] [varchar](9) NULL,
[con_first_name] [varchar](50) NOT NULL,
[con_last_name] [varchar](50) NOT NULL,
[payer_Addr_line1] [varchar](100) NULL,
[payer_Addr_line2] [varchar](100) NULL,
[payer_city] [varchar](100) NULL,
[payer_state] [varchar](50) NULL,
[payer_zip] [varchar](50) NULL,
[payer_phone] [varchar](50) NULL,
[con_designation] [varchar](50) NULL
Credentials
CREDENTIALS
[cred_id] [int] IDENTITY(500000,1) NOT NULL,
[cred_company_id] [int] NULL,
[cred_clientID] [varchar](50) NOT NULL,
[cred_clientSecret] [varchar](50) NOT NULL,
[cred_created_at] [datetime] NULL,
[cred_updated_at] [datetime] NULL,
[cred_updatedby_id] [int] NULL,
[cred_is_active] [bit] NULL,
[cred_con_email] [varchar](60) NULL
Prior Authorization
Prior Authorization dashboard
The following columns are included in the dashboard
DDDID preAuth table
Patient Name cus_name from customer table using DDDID
Patient Last Name Remove this column from the dashboard
Patient DOB customer table using DDDID
Medicaid ID preAuth table
Prior Authorization preAuth table
Procedure Code preAuth table
Diagnosis Code PrimaryDiagnosisCode ‘:’ SecondaryDiagnosisCode from
customer table using DDDID
Task Start Date preAuth table
Task End Date preAuth table
Authorized Units preAuth table
Authorized Amount preAuth table
Total Charges Same as Authorized Amount
Claim Status WILL BE UPDATED BY BILLING PROCESS (Siddarth)
MMT
Response Status WILL BE UPDATED BY BILLING PROCESS (Siddarth)
Created Date tas_created_at from task table, as identified below
Last Response Date WILL BE UPDATED BY BILLING PROCESS (Siddarth)
Error Code preAuth table
Error Description preAuth table
Matching task to Prior Auth
Identify tas_id from the task table by first identifying an active project for the given customer. If there are multiple active projects, pick the first one.
Use this project ID to find a task from task table, where tas_pro_id is this project ID, and tas_is_active = 1, and tas_start_date is between Task Start Date and Task End Date and tas_mm_id is not null
Last updated