💳Revenue Cycle Management
Billing can become a labor-intensive process. Tracking down the relevant documentation, figuring out the amount of time spent on visits and other activities, and spotting errors. Fieldworker can help.

Track time with ease Whether you’re in the office or the field, on a computer, tablet or cellphone, FieldWorker has made it simple to accurately track your time wherever you are. Simply check in and out for any activity to clock in exactly the right number of hours.

Automate quality controls
Fieldworker contains all of your records and documentation in one easy-to-access place. You’ll have the information you need for billing at your fingertips – and thanks to precise tracking, you can rely on the fact that it’s up-to-date and correct.

Eliminate billing errors, hello faster payments
By ensuring your data is accurate, you can be confident that your bills are correct. You spend less time resolving issues among you, clients and insurers, and achieve an overall faster payment cycle. Less time wasted, faster payments – it’s a win-win!
How Does the Revenue Cycle Work?
The Revenue cycle is the financial process related to a patient's clinical or non-clinical encounter. It includes obtaining proof of service delivery, ensuring that the prior authorization of the services is already in place, submitting the accurate claim, reconciling the remittances, and following up on accounts receivable while maintaining compliance with payer, federal, and/or state regulators.
The fieldworker sets you up to submit your claims to Medicaid (or other payers). In New Jersey, as an agency, you’ll sign up for NJMMIS through us so that we’ll be able to submit your claims electronically through FieldWorker. Our team will guide you through this process when you sign up.
There are two different pathways to submit claims to Medicaid.
An agency can manage the entire Revenue Cycle within the Fieldworker app. In this case, Fieldworker is used to manage all your population, and associated authorizations, track services, and then match services provided with the prior authorizations in the system to generate claims, or
An agency can submit a prepared file containing claims data in CSV format instead of manually submitting it through the CMS-1500 form.
Revenue Dashboard
The Fieldworker presents a dynamically updated revenue dashboard showing expected cash flow and its status, including authorization, service delivery, claims, and remittances.

Claims - Basics
Any claims submitted by noon each Friday will be submitted to NJMMIS within that week. For all valid accepted claims, you’ll receive payment the following week. The payment information will be available via the remittance files received from NJMMIS.
If there are any issues with the claim, including denials or further information needed, the submitted claims may be tracked within the Fieldworker dashboards and/or reports. Once resolved, the claim can be resubmitted through FieldWorker.
Prior Authorization
To ensure that the service provider or SDE can receive payment for the services they are providing, prior authorization must be obtained BEFORE the service is delivered. Services begun or provided without prior authorization or outside of the scope of the prior authorization will not be reimbursed. Medicaid must receive prior authorization from the Division before it will remit payment for a claim.
If you run a service provider agency
Prior authorizations are created upon approval (or modification) of the ISP and automatically generated for each week of service. A secure email containing the approved ISP and a Service Detail Report detailing the start/end dates, number of units, and procedure codes for services authorized for delivery is automatically generated and sent to all identified service providers and/or the FI in circumstances when the individual is utilizing an SDE or accessing a waiver service through a business that is not a Medicaid provider.
Medicaid sends a letter to providers whenever a prior authorization is created, changed, or revoked. The most recent prior authorization supersedes any previous prior authorizations. Without prior authorization, it is possible that a claim will not be paid.
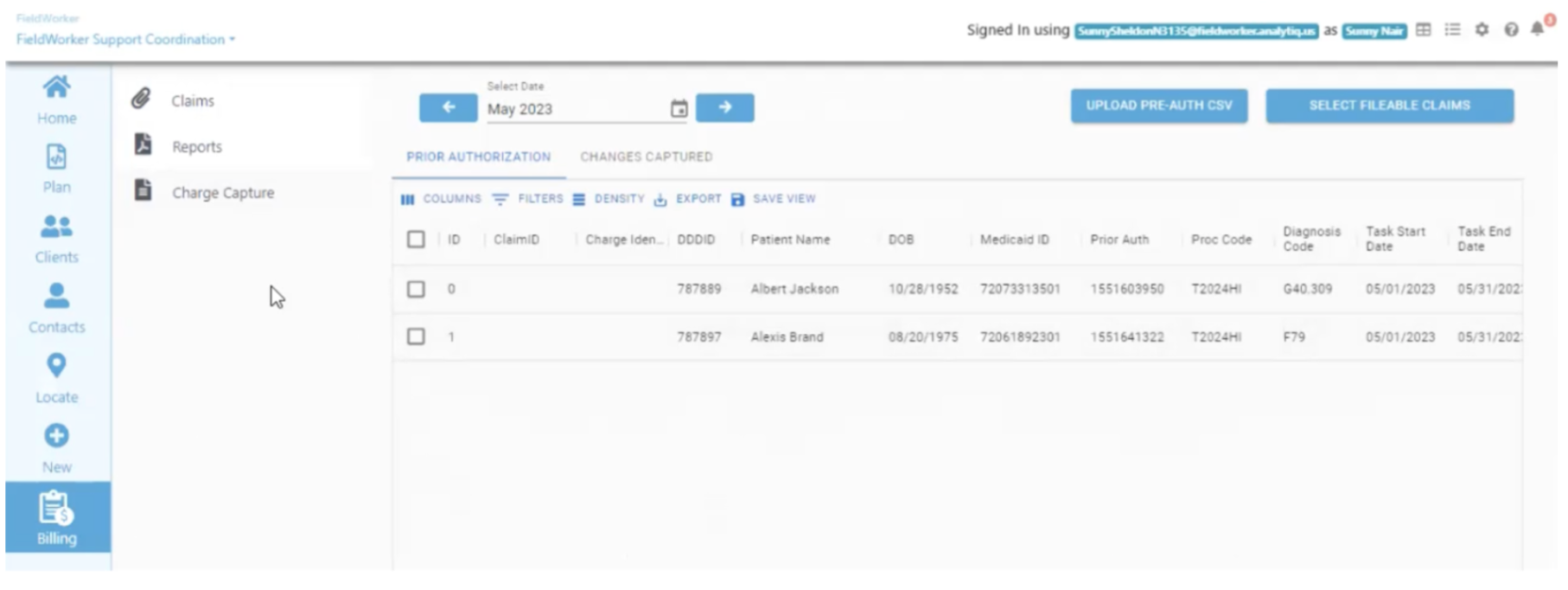
Fieldworker lets you upload your Pre Auth CSV or lets you create a detailed weekly schedule for each client using the SDR received from the Support Coordinator. You upload this file by clicking on the “Upload Pre-Auth CSV” in the top right of this screen (under Billing and “Charge Capture” from the side panels).
Patient encounters or Services provided
Documentation of the delivery of all services must be maintained to substantiate claims. This documentation should include the date, start and end times, and the number of units of the delivered service for each individual. The services delivered must align with the prior authorization received for the provision of services and the individual’s ISP.
If your agency is managing customers, Plans, and Services within Fieldworker, Your services delivered may be automatically matched against the authorizations. Specific matching logic used by the Fieldworker is explained in the specific Use Cases discussed elsewhere.
Accounts Receivable
For New Jersey, Support Coordination businesses that opt for 'Financial Reporting' functionality, the Fieldworker automatically generates billables to produce accounts receivable. The billables are created at the beginning of each month, as well as whenever a change is detected. See the above page for accounts receivable accounting logic used for the creation of accounts receivable entries.

Charge Recognition
The following factors must be in place in order to generate a claim for a Medicaid service:
The delivery of service must be properly documented, along with any delivery documents necessary to substantiate the claim in the case of an audit. Services may have specific deliverable documents (such as Tools, timesheets, and/or behavior plans) relevant to the delivery of that service.
The service that was provided must have a valid prior authorization, and
The claim must include participant information and service information (such as Medicaid ID, diagnosis, procedure code, rate, etc.), which can be found within the service plan and service detail report.
Rounding of Service Units
Providers are allowed to add non-continuous units of billable visits together. This requires careful documentation supporting the time the individual sessions were provided. These times may not be estimated. The provider may then add non-continuous units together to reach a total. Since units are 15 minutes in length, the initial unit of service less than 15 minutes may be billed as one unit. Beyond the initial unit, service times less than half of the unit shall be rounded down while service time equal to or greater than half shall be rounded up.
Unit Accumulation
Prior authorized units of service that have not been utilized can carry over for future use within the ISP plan year as long as the service and provider that were prior authorized remain the same. If prior authorized units of service are not utilized, due to an unscheduled absence, unexpected program closure, lack of need for that service that particular week, etc., the service provider or SDE remains prior authorized to provide those carryover units at any time within the ISP plan year.
Fieldworker help Service providers and SDEs track units used compared to units authorized in order to ensure payment for all services rendered.
The Fieldworker may be matching services offered by your agency to a prior authorization if you are either a Support Coordination agency or a Care Provider agency. The fieldworker ensures proper adherence to all three factors. Billing claims are created through the prior authorization form you receive from the DDD at the start of every month. Claims matched via Automatic Charge recognition can be generated and submitted from the Prior Auth screen on the Billing Dashboard.

Charge Capture
The charge capture screen has inbuilt logic to mine changes in prior authorizations where external events may have caused pre-existing prior authorizations to change. In such cases, Fieldworker lets you ensure that no charges are missed and are correctly filed.

This screen also captures events that may not have been captured in a single authorization file. Such events may include acquiring a new customer, losing a customer, or changes in the plan in the middle of the month.
If an authorization is included in the latest authorization file but was not in last month's file, the change (New customer) is captured, and a claim for the partial month will be generated.
If an authorization is not included in the latest authorization file but was in last month's file, the change (Customer leaving) is captured, and a claim for the partial month will be generated. The end date for the partial claim will be taken from the Fieldworker's internal records.
If the authorization entry is changed between any two prior authorization files, the change (Plan changes) is identified, and two or more partial submissions are generated.
For a task that has approved documentation but lacks prior authorization, the task will be logged. The user may then generate a claim for a partial month if the plan is approved but unsigned by the consumer.
Billing Dashboard
Under “Prior Authorization”, you can see all prior authorizations received in the system. They may have been uploaded directly, as received from DDD or other agencies, or may have been generated using the detailed Service Delivery Report.
Under 'Claims', you can see all claims that are either directly uploaded into the system or may have been sent via prior authorization matching. For exact matching logic, please see the relevant use cases. The claims dashboard also executes a suite of validations to ensure error-free submission to Medicaid.
Under “Changes Captured”, you’ll see any changes made from the previous month when uploading your pre-authorization.
Uploading Claims
If your agency has not yet been set up for a complete Revenue Cycle, you may upload your claims using a proprietary CSV file.

Claims Dashboard
You’ll then see your claims for billing updated here.
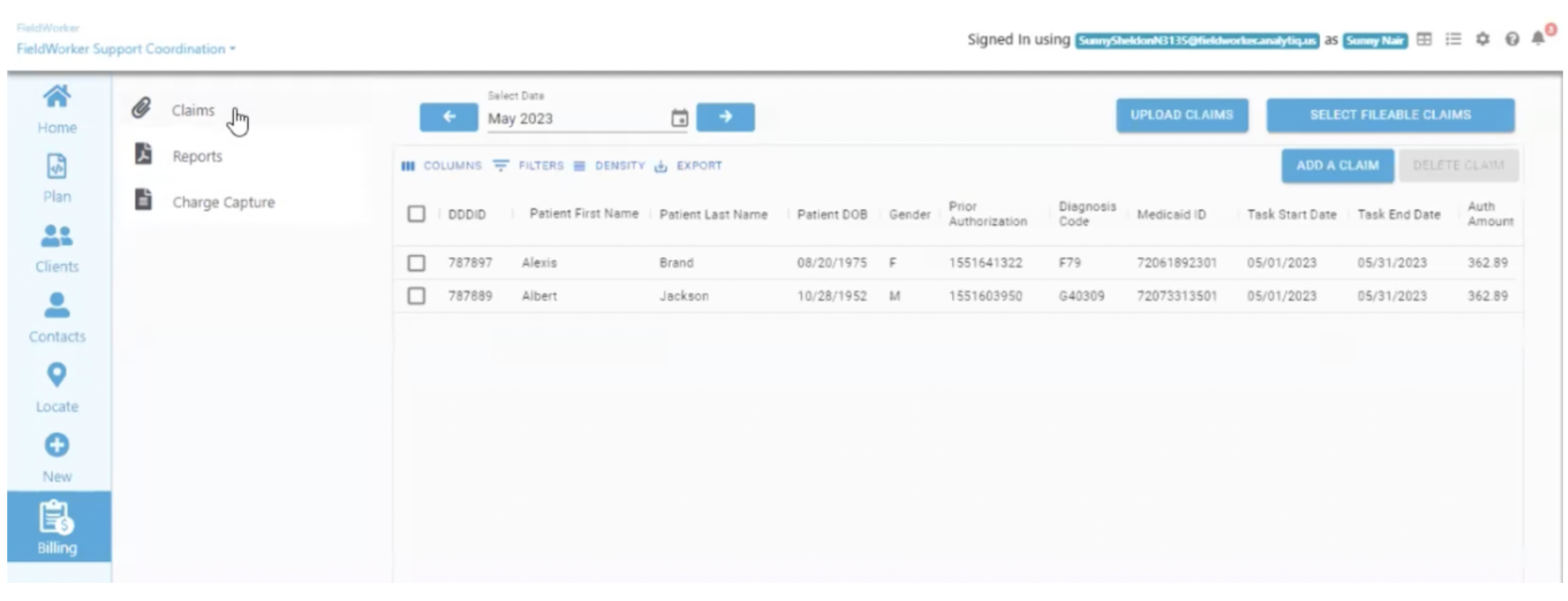
Once uploaded, the claims dashboard will show all the claims, and it will also highlight if there are any formatting issues.
The following validations are performed for all submitted claims.
Diagnosis Code:
should only contain alphanumeric characters
if multiple diagnosis codes are present, use a forward slash or '/' to separate them
Procedure Code and Procedure Code Modifiers
should only contain alphanumeric characters
if multiple procedure code modifiers are present, use a colon ':' or a forward slash '/' to separate them
First Name and Last Name
should only contain alphabets, commas, periods, hyphens, and single quotation marks
You can check the issue in the error column. Almost every field is editable, so the user can edit it in place to update the field to the correct value. If a claim satisfies all validations, it will be marked as 'Ready to Bill', and can be submitted for billing.

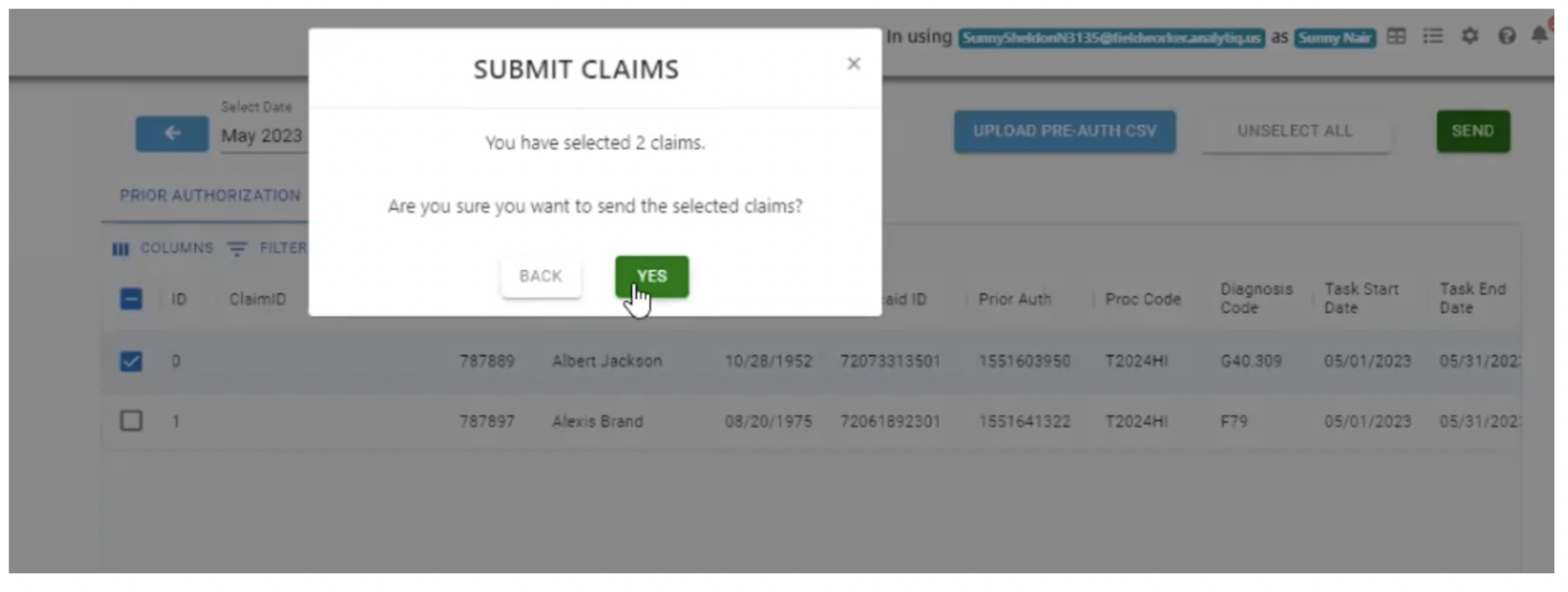
Submitting Claims
In order to submit your claim, go to “Billing”, and then “Claims” to see any claims which are marked as “Ready to bill”. Select the checkbox for the row for the claims you wish to submit, and click the green “Send” button in the top right. You’ll only see this button if you have selected a claim eligible for submission.
You’ll then be shown a pop-up asking you to confirm that you would like to submit the selected claims. Click “Yes” to confirm.
Claims Processing
The claims will be submitted after confirmation from the user. Once submitted, the user is not allowed to edit any field.
In a few hours, the user will get an update about the submission, which will be shown in the status column.
If the claim is denied at this stage, the user should look at the error and edit the claim accordingly to make it correct and resubmit it.
NJMMIS processes all claims submitted from Monday to Friday on the upcoming Monday. So the statuses of the claims will once again be updated on Monday Morning around 10 am EST.
If the claims are denied here, there will be an associated error code and an error description, through which the user can correct it and resubmit it.
Private Payer Billing
Documentation to be added
Billing Reports
Outstanding Balance Report
The report shows claims submitted that have not yet been paid off.

Claim Balance Report
This report shows the aging of the unpaid claims.

Claim Collection Report
This is relevant if your practice supports multiple sources of payment for services provided.

Billing Transaction Report
This report shows the details of all outstanding claims.

Last updated